1. Principles
General remarks
Fixation of proximal humeral fractures is frequently associated with problems related to the healing of the tuberosities and/or the humeral head fragment. If the tuberosities heal in a grossly displaced position the clinical outcome is poor and may require further surgery. For this reason, reverse shoulder arthroplasty is an attractive option in elderly patients. Since this kind of shoulder replacement does not rely on the function of the rotator cuff, it provides predictable results in terms of pain relief and shoulder function in one operation.
Indications
The indications for reverse shoulder arthroplasty in proximal humeral fractures are still not clear. Recent published clinical results suggest a growing spectrum of indications. The classic indication was a displaced four-part fracture in an elderly patient, especially if the tuberosities are comminuted or very small avulsion fractures. More recently, under such conditions, even three- and two-part fractures may be considered.
Keys to successful reverse shoulder arthroplasties
- Correct determination of the surgical landmarks
- Extensive soft tissue release
- Proper determination of prosthesis size and version
- Proper height of the prosthesis with correct soft-tissue tensions
- Stable fixation of the tuberosities to promote their union to the proximal humerus
2. Patient preparation and approaches
Patient preparation
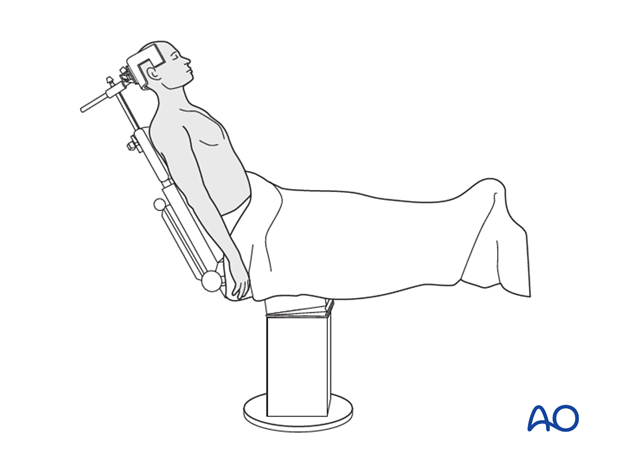
It is recommended to perform this procedure with the patient in a beach chair position.
Alternatively the patient may be positioned supine if the procedure is converted from ORIF.
Recommended approach
The deltopectoral approach is recommended.
The anterolateral and transdeltoid lateral approach can be used but are not recommended because of:
- Risk of axillary nerve injury
- Risk of deltoid muscle injury
3. Evaluation of the fracture
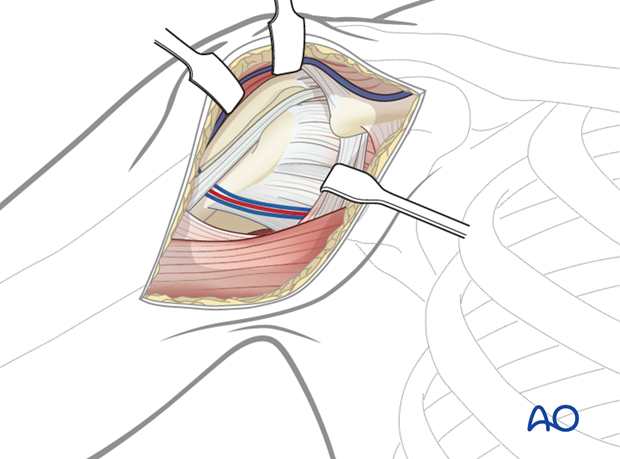
It is crucial to evaluate the fracture. Identify the fracture lines, the long head of the biceps and the condition of the rotator cuff.
4. Tenotomy of the long head of the biceps
The biceps tendon may be attached to the superior border of the pectoralis major with a simple suture. Perform a tenotomy of the long head of the biceps close to the rotator interval.
Pearl: Move the stump of the biceps tendon out of the surgical field.
5. Surgical technique for two- or three-part fracture
Principles
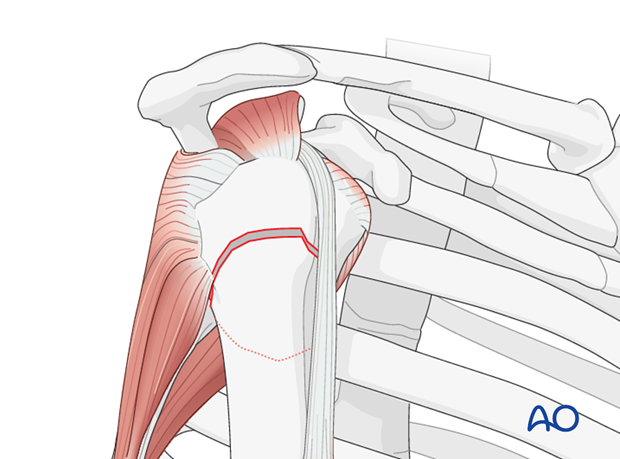
The greater and lesser tuberosities must be isolated and free of cartilage. The subscapularis tendon and the infraspinatus tendon should be mobilized and secured with a stay suture. The supraspinatus tendon should be excised.
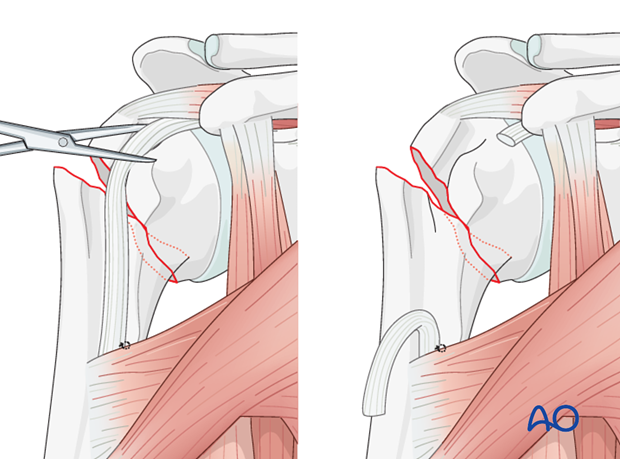
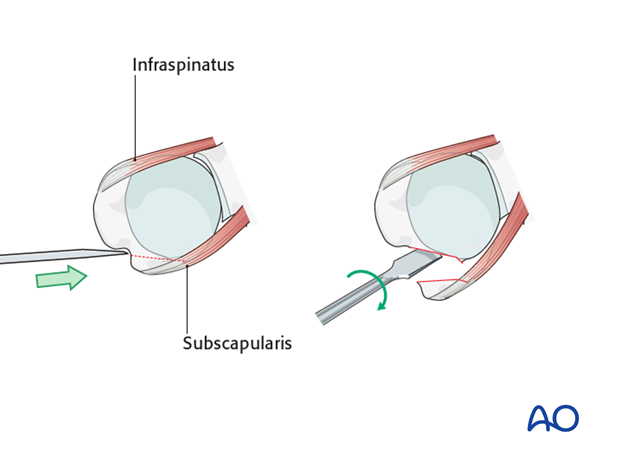
Osteotomy of the lesser tuberosity
If the lesser tuberosity is still attached it must be detached.
Incise the rotator interval with scissors.
Perform an osteotomy of the lesser tuberosity; start at the deepest point of the bicipital groove. Crack the lesser tuberosity off with a gentle twist of the osteotome. Incise the remaining anterior capsule and release the lesser tuberosity. Remove any remaining cartilage if present.
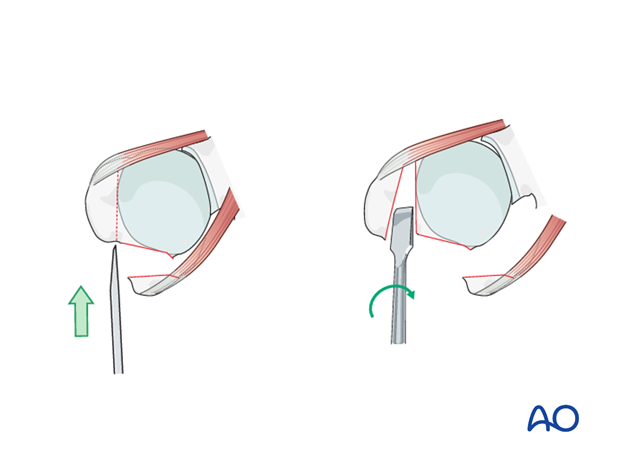
Osteotomy of the greater tuberosity
If the greater tuberosity is still attached it must be detached.
Perform an osteotomy of the greater tuberosity. Again, start at the deepest point of the bicipital groove and tilt the osteotome posteriorly parallel to the greater tuberosity. Crack the greater tuberosity off with a gentle twist of the osteotome. Incise the remaining posterior capsule and release the greater tuberosity. Remove any remaining cartilage if present.
6. Preparation of the joint for placement of prosthesis
Retrieve the humeral head
Any remaining medial capsular attachment to the head should be carefully released, paying special attention not to damage the axillary nerve medial to the proximal humerus.
Be sure that all loose small fragments are removed.

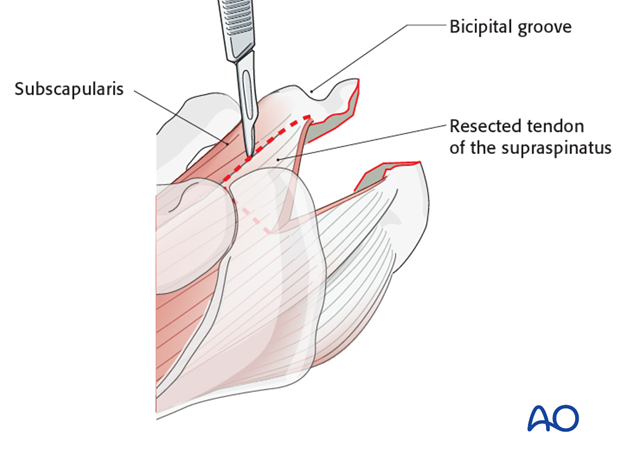
Mobilization and preparation of the lesser tuberosity
Resect the anterior part of the supraspinatus tendon and the rotator interval up to the superior border of the subscapularis tendon. Remove all scar tissue around the subscapularis tendon. Remove adjacent cartilage if remaining. Secure the subscapularis tendon with a stay suture.
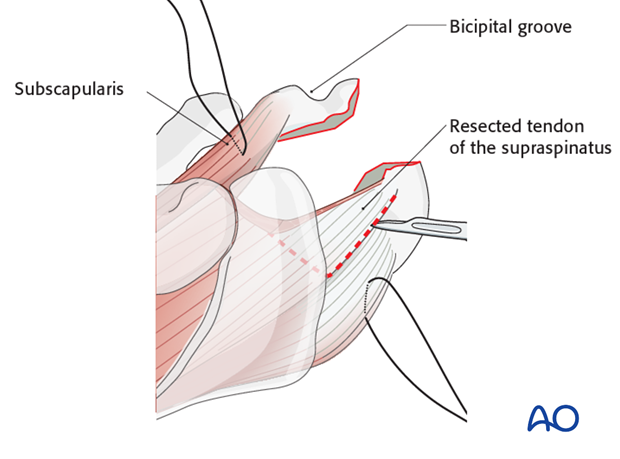
Mobilization and preparation of the greater tuberosity
Resect the posterior part of the supraspinatus tendon up to the superior border of the infraspinatus tendon. Mobilize the infraspinatus tendon and secure it with a stay suture. Remove adjacent cartilage of the greater tuberosity if remaining.
Exposure of the glenoid
Expose the glenoid between retractors which are placed at the anterior and posterior rim of the glenoid.
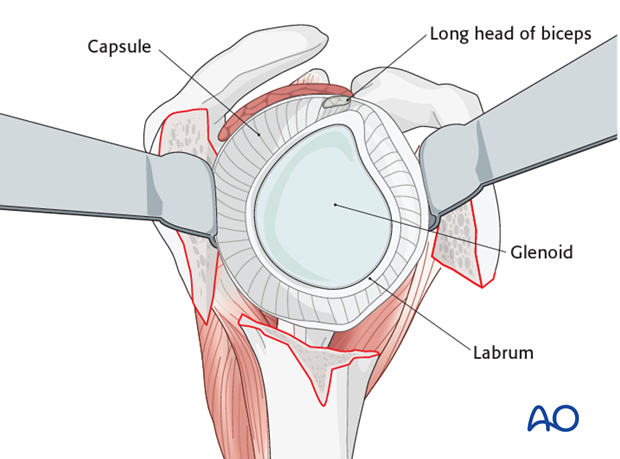
Glenoid-sided soft-tissue release
Perform a complete soft-tissue release around the glenoid. Start with the resection of the anterosuperior labrum including the remnants of the biceps. Continue with an anterior, inferior and later posterior release. Place retractors at the anterior, inferior and posterior rim of the glenoid.
Inspect the glenoid fossa in order to rule out any additional injury.
If there is a glenoid fracture, osteosynthesis should be performed now.
Remove any bony fragments.

7. Glenoid surgical steps
General remarks
For reverse shoulder arthroplasty, various prosthetic systems are available.
The principles of the procedure are shown here on a representative example of one system. For detailed information, refer to the manufacturer’s manual.
Glenoidal preparation
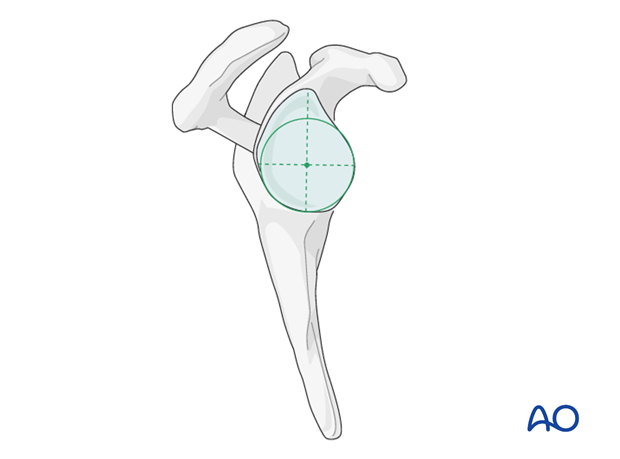
Place the guide plate on to the glenoid surface so that it is flush with the circle of the lower glenoid (green line). Fix the guide plate with a central K-wire.
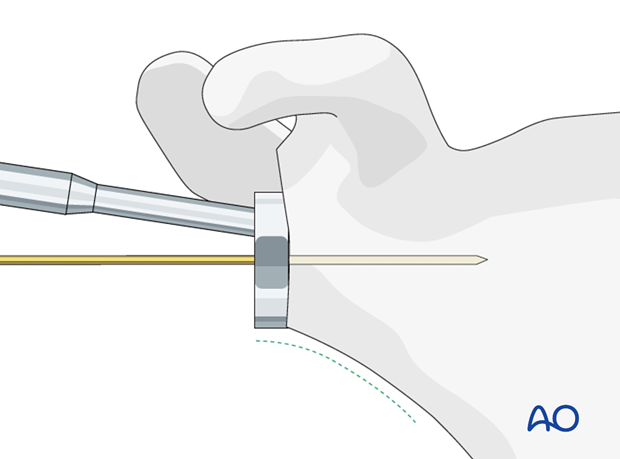
The K-wire (and therefore later the central peg) should be positioned in the center of the inferior circle of the glenoid.
Control the position of the K-wire with preoperative planning including radiographic and CT images.
Use a cannulated glenoid resurfacing reamer to remove the cartilage and to create a smooth surface of the glenoid to provide full contact with the base plate.
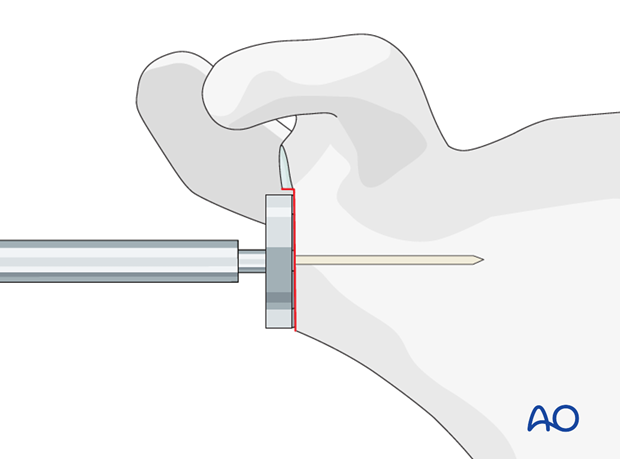
Extend the glenoidal preparation superiorly with an additional cannulated surface reamer to assure later pressfit fixation of the glenosphere to the base plate without any bony or soft-tissue impingement.
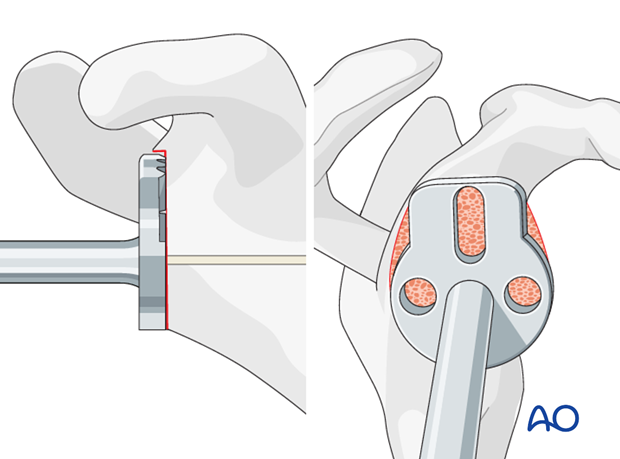
Drill the hole for the central peg using a cannulated drill.
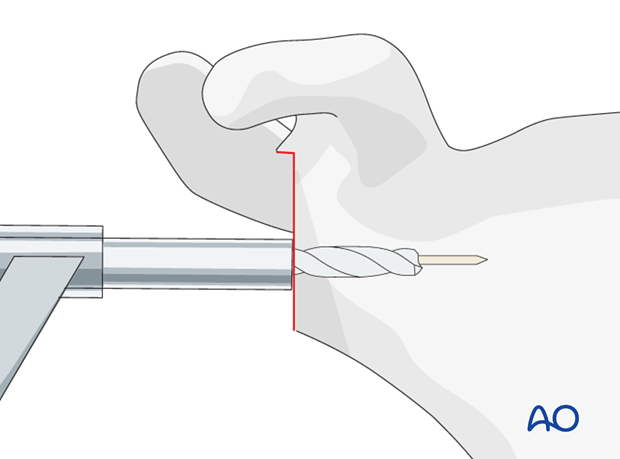
Align the base plate and implant it with gentle taps of a mallet.
Fix the base plate with screws according to the manufacturer’s manual.
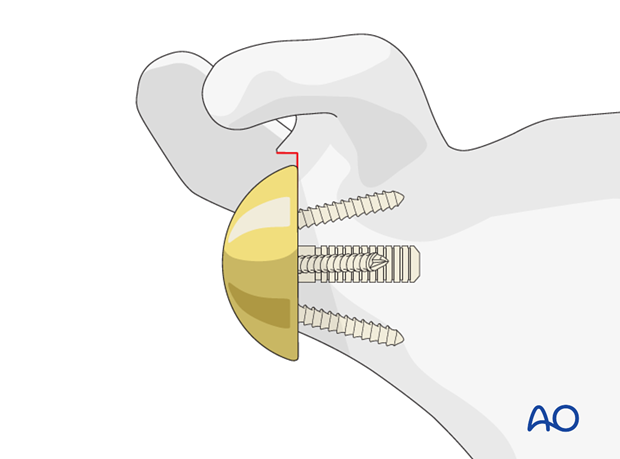
Glenosphere implantation
Implant the glenosphere. A trial glenosphere may be used instead of the definitive one.
Note: The size of the glenosphere should be bigger than the AP diameter of the glenoid in order to prevent impingement. The glenosphere should also have a slight inferior overhang in order to minimize the risk of inferior notching.
8. Humerus surgical steps
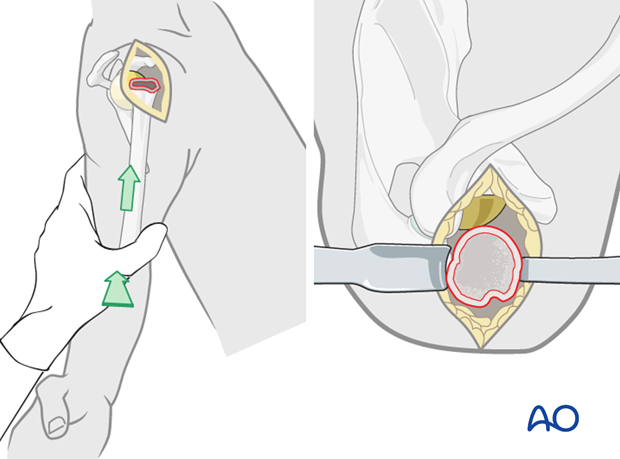
Exposure of the proximal humerus
Expose the proximal humerus with retroflexion and adduction of the humerus so that the fracture plane lies in front of the glenosphere. Additional upwards pushing is helpful. Anterior and posterior retractors placed behind the proximal humerus may improve the exposure.
Preparation of the intramedullary canal
Prepare the intramedullary canal with reamers of increasing diameters until the cortical bone of the humerus is reached. Take care to be gentle in osteoporotic bone in order to prevent iatrogenic fractures.
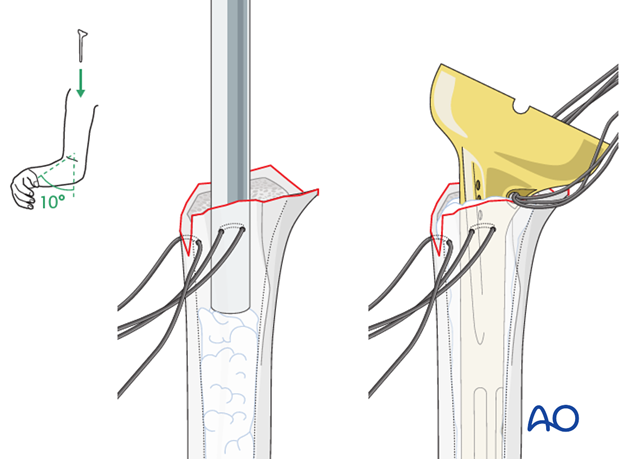
Placement of a humeral trial prosthesis
Insert the humeral trial prosthesis determined by the size of the last reamer.
Mount a standard trial inlay according to the size of the glenosphere. There is some debate about the ideal retrotorsion of the prosthesis. We recommend a retrotorsion of 10°.
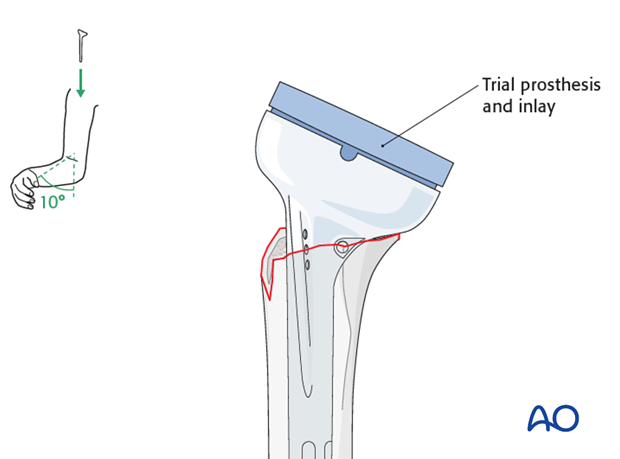
Reduction and assessment of joint tensioning and stability
Reduce the prosthesis and confirm proper joint tension and stability. Do not overtension the deltoid muscle. Check if there is any unwanted impingement.
If necessary repeat this step with different inlays.
Mark the position of the trial implant in relation to the humerus.
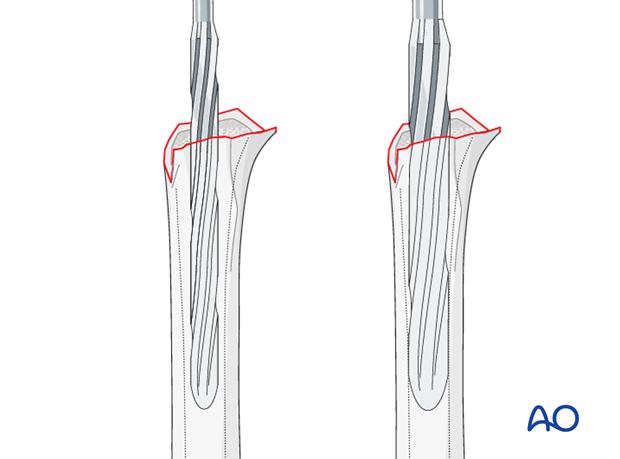
Preparation of the humerus for cementing
Expose the proximal humerus again and prepare the intramedullary cavity with pulsed lavage and a medullary canal stopper.
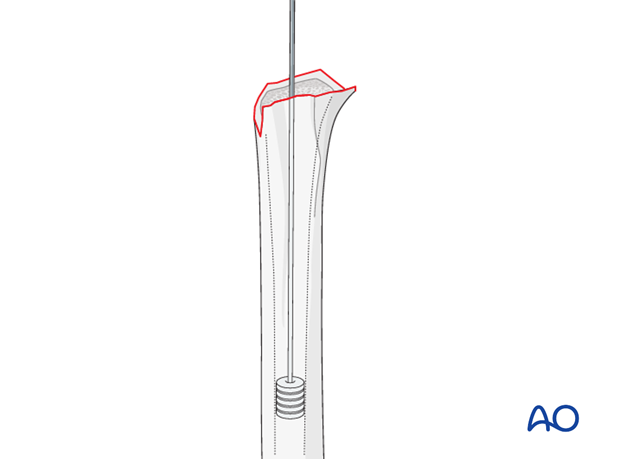
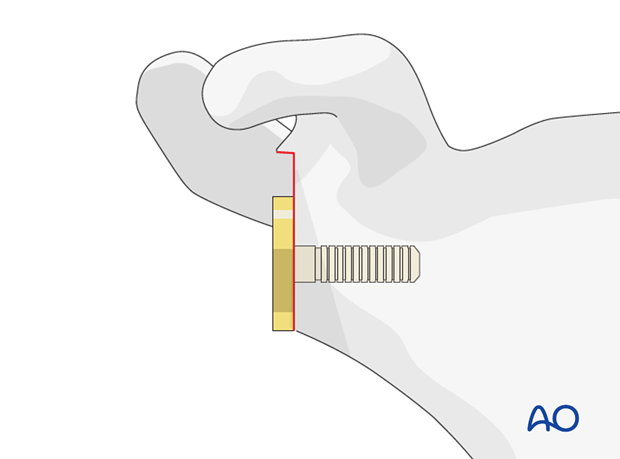
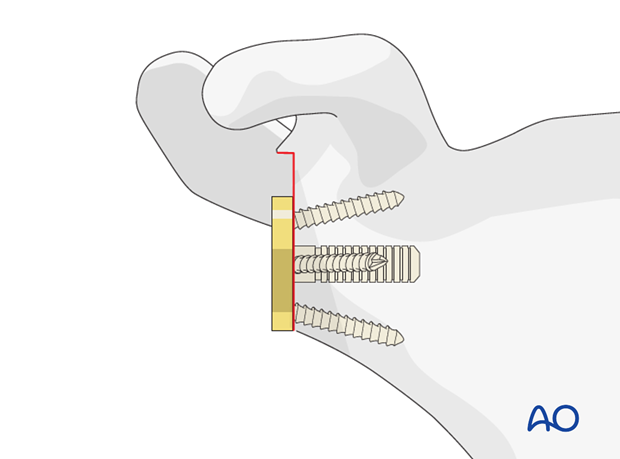
Drill two 2.0 mm holes through the humeral shaft on each side of the bicipital groove and pass a heavy, non-resorbable suture through each side.

Pass three heavy, non-resorbable sutures through the infraspinatus tendon, the medial suture hole of the definitive prosthesis and the subscapularis tendon. These sutures will help to fix the tuberosities to the prosthesis later.

Implantation of the definitive prosthesis
Typically, a cemented fixation of the definitive prosthesis is necessary.
Cement the prosthesis in the previously chosen position in respect to the prosthesis height and retrotorsion.
After hardening of the cement, insert the chosen inlay and reduce the prosthesis.
Confirm correct soft-tissue tension and stability.
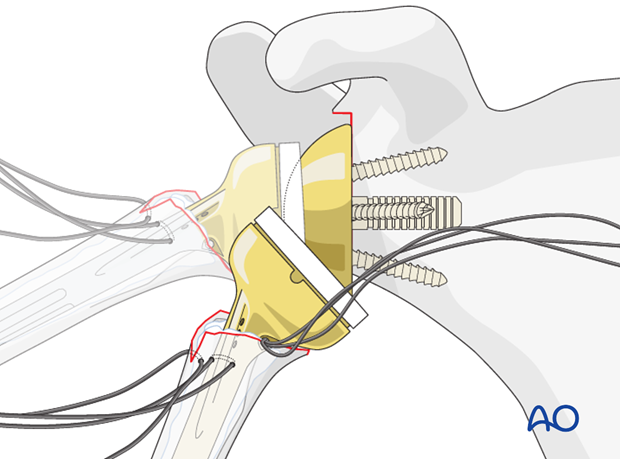
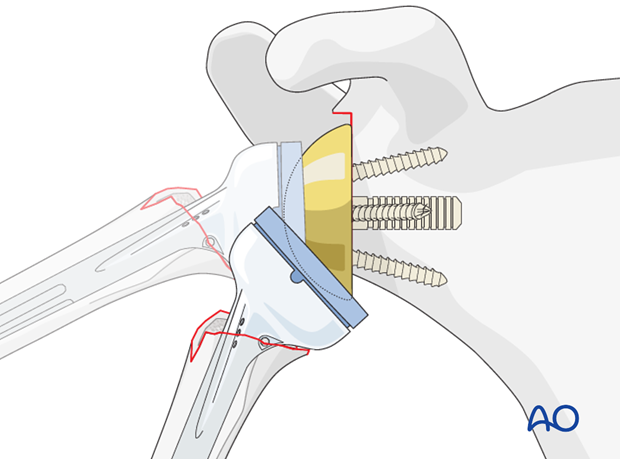
9. Fixation of the tuberosities
Reduce the tuberosities so that they have contact with the humeral shaft. A slight overlap ensures better bony healing of the tuberosities.
Start with tying the three horizontal sutures embracing the tuberosities around the prosthesis.
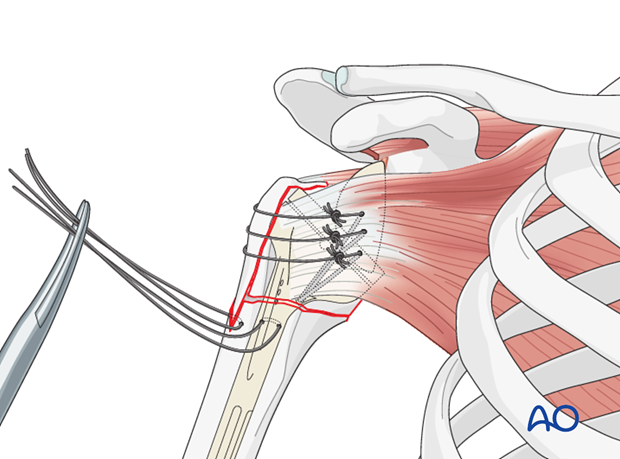
Pass the prepared sutures from the humeral shaft through the infraspinatus and the subscapularis tendon and tie the sutures, in order to prevent a superior dislocation of the tuberosities.
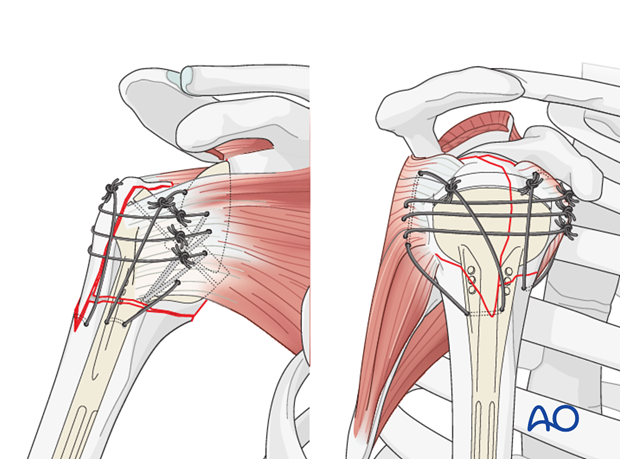
Confirm the final position of the tuberosities and the position of the implants with an image intensifier. Take care to obtain a true AP projec


