Intramedullary and Dorsal Plate Fixation of Distal Radius Fractures
Intramedullary and Dorsal Plate Fixation of Distal Radius Fractures
DEFINITION
ANATOMY
PATHOGENESIS
NATURAL HISTORY
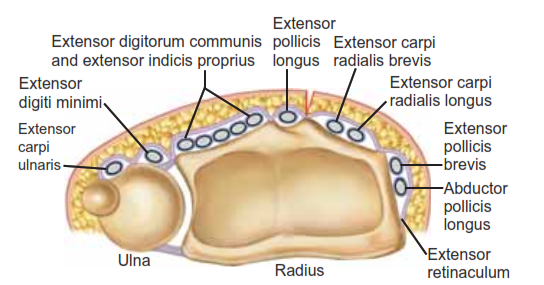
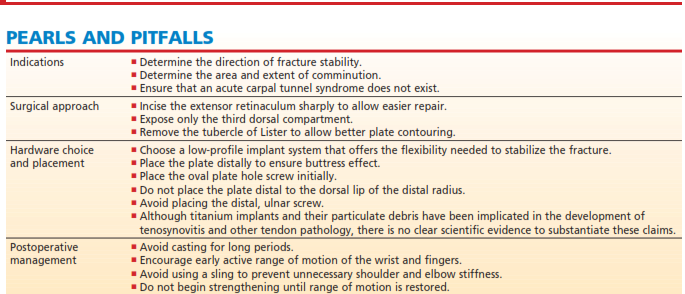
FIG 1 • Anatomy of the distal radius. The six dorsal extensor compartments at the level of the extensor retinaculum.
PATIENT HISTORY AND PHYSICAL FINDINGS
IMAGING AND OTHER DIAGNOSTIC STUDIES
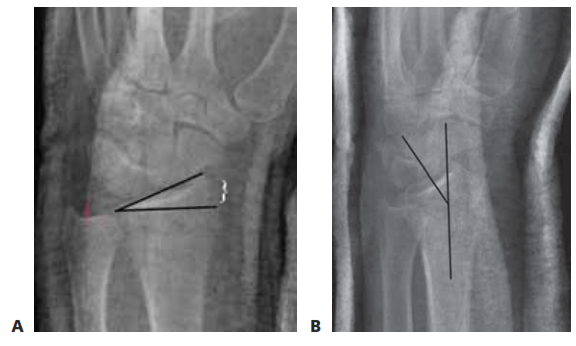
FIG 2 • A. PA radiograph demonstrating radial inclination, (black lines), ulnar variance (red), and radial height (white bracket). 8. Lateral radi- ograph of the wrist demonstrating volar tilt (black lines).
DIFFERENTIAL DIAGNOSIS
NONOPERATIVE MANAGEMENT
SURGICAL MANAGEMENT
Preoperative Planning
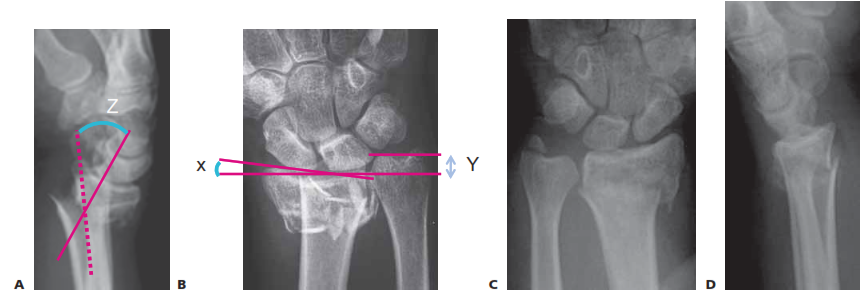
FIG 3 • PA radiograph (A) and lateral radiograph (B) of a healed distal radius fracture fixed with an intramedullary plate. C,D. PA and lateral radiographs showing an unstable metaphyseal distal radius fracture. (C,D: copyright Thomas R. Hunt III, MD.)

FIG 4 • Patient is positioned supine with arm on a hand table and tourniquet applied on proximal arm.
DORSAL PLATE FIXATION OF DISTAL RADIUS FRACTURES
Incision and Dissection

TECH FIG 1 • A. Skin incision is drawn in relation to the tubercle of Lister. B. Skin incision is carried down to extensor reti- naculum. Tubercle of Lister and retinacular incision are drawn. C. The retinaculum is incised and the EPL tendon is exposed. Hematoma has already been evacuated. (continued)
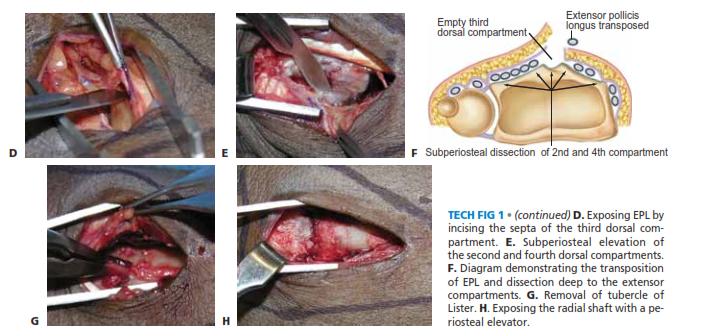
TECH FIG 1 • (continued) D. Exposing EPL by incising the septa of the third dorsal com- partment. E. Subperiosteal elevation of the second and fourth dorsal compartments. F. Diagram demonstrating the transposition of EPL and dissection deep to the extensor compartments. G. Removal of tubercle of Lister. H. Exposing the radial shaft with a pe- riosteal elevator.
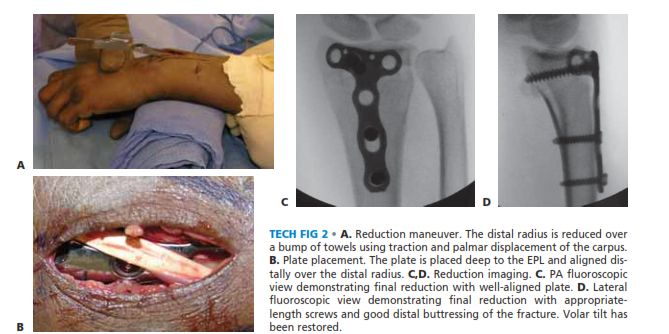
TECH FIG 2 • A. Reduction maneuver. The distal radius is reduced over a bump of towels using traction and palmar displacement of the carpus. B. Plate placement. The plate is placed deep to the EPL and aligned dis- tally over the distal radius. C,D. Reduction imaging. C. PA fluoroscopic view demonstrating final reduction with well-aligned plate. D. Lateral fluoroscopic view demonstrating final reduction with appropriate- length screws and good distal buttressing of the fracture. Volar tilt hasbeen restored.
Wound Closure
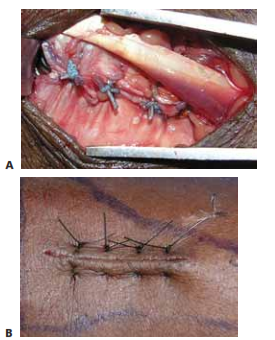
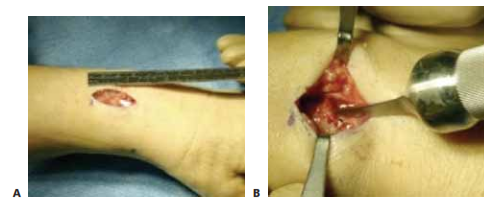
TECH FIG 3 • A. Retinacular closure. The extensor retinaculum is closed deep to the EPL with a nonabsorbable suture. B. Skin closure. The skin is closed with a horizontal mattress stitch toevert the skin edges.
FIXATION OF DISTAL RADIUS FRACTURES USING A DORSAL INTRAMEDULLARY DEVICE (TORNIER)
TECH FIG 4 • A. A 2.5-cm dorsal incision is used for exposure. B. The awl is inserted through the fracture site after removal of the tubercle of Lister. (continued)

TECH FIG 4 • (continued) C. A rasp is used to create a path for the implant. D. The implant is placed using the insertion device so as to control rotation during seating. E,F. An un- stable metaphyseal distal radius fracture has been reduced and stabilized using a dorsal intramedullary device (TornierCorp). (E,F: copyright Thomas R. Hunt III, MD.)
FIXATION OF DISTAL RADIUS FRACTURES USING A RADIAL INTRAMEDULLARY DEVICE (WRIGHT MEDICAL)
PEARLS AND PITFALLS