Femoral Neck Fractures
Open Reduction and Internal Fixation and Closed Reduction and Percutaneous Fixation of Femoral Neck Fractures
DEFINITION
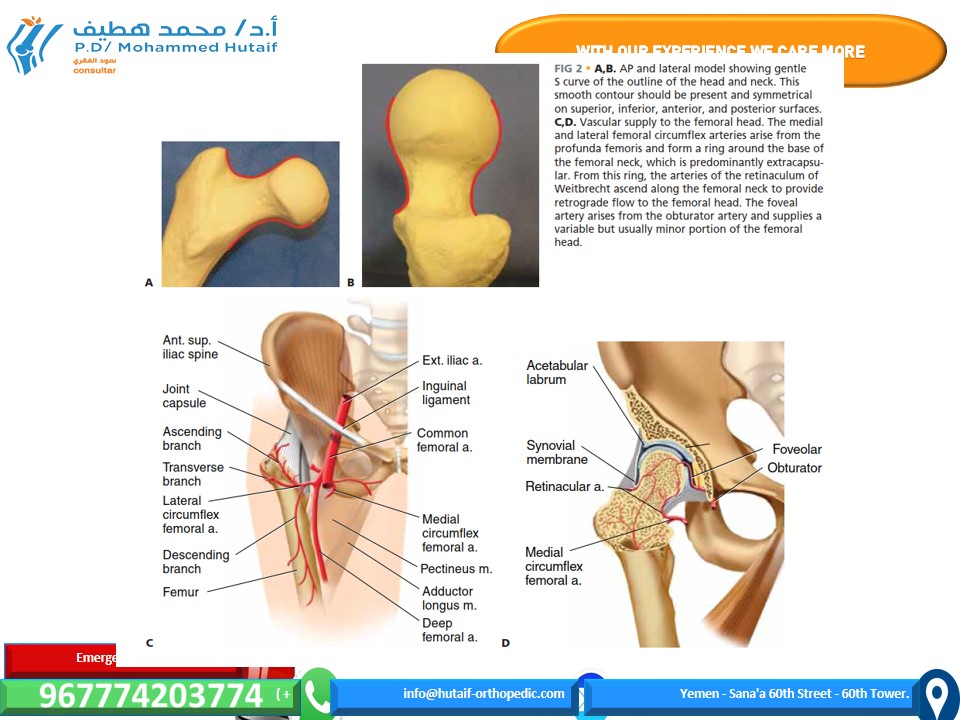
ANATOMY

PATHOGENESIS
NATURAL HISTORY
PATIENT HISTORY AND PHYSICAL FINDINGS
IMAGING AND OTHER DIAGNOSTIC STUDIES

DIFFERENTIAL DIAGNOSIS
NONOPERATIVE MANAGEMENT
SURGICAL MANAGEMENT
Preoperative Planning
Positioning

Approach
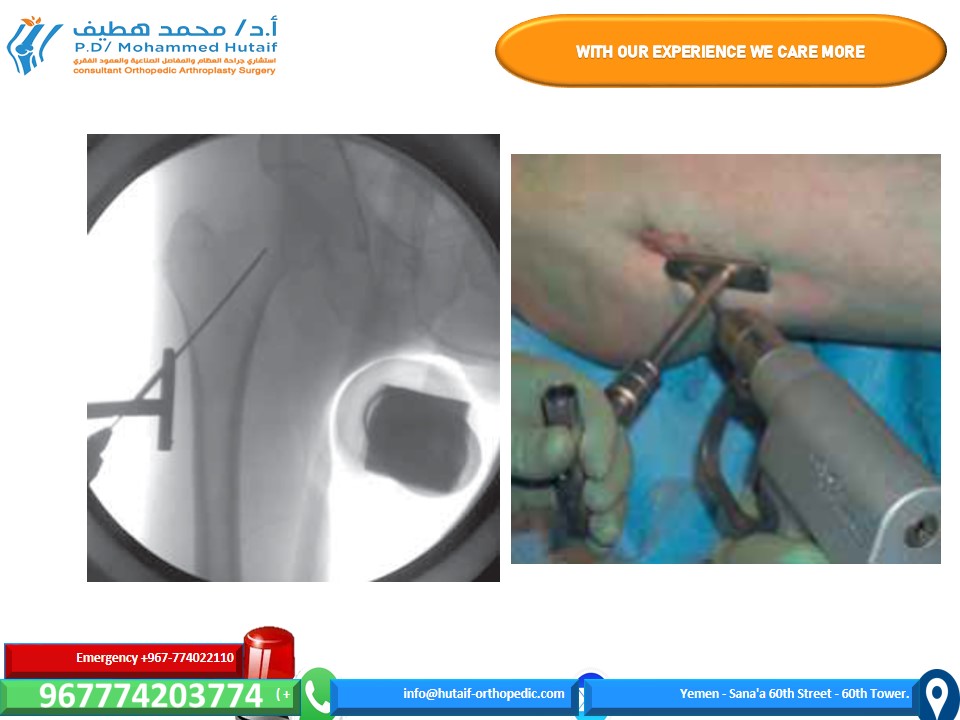
CLOSED REDUCTION AND PERCUTANEOUS FIXATION

Arthrotomy
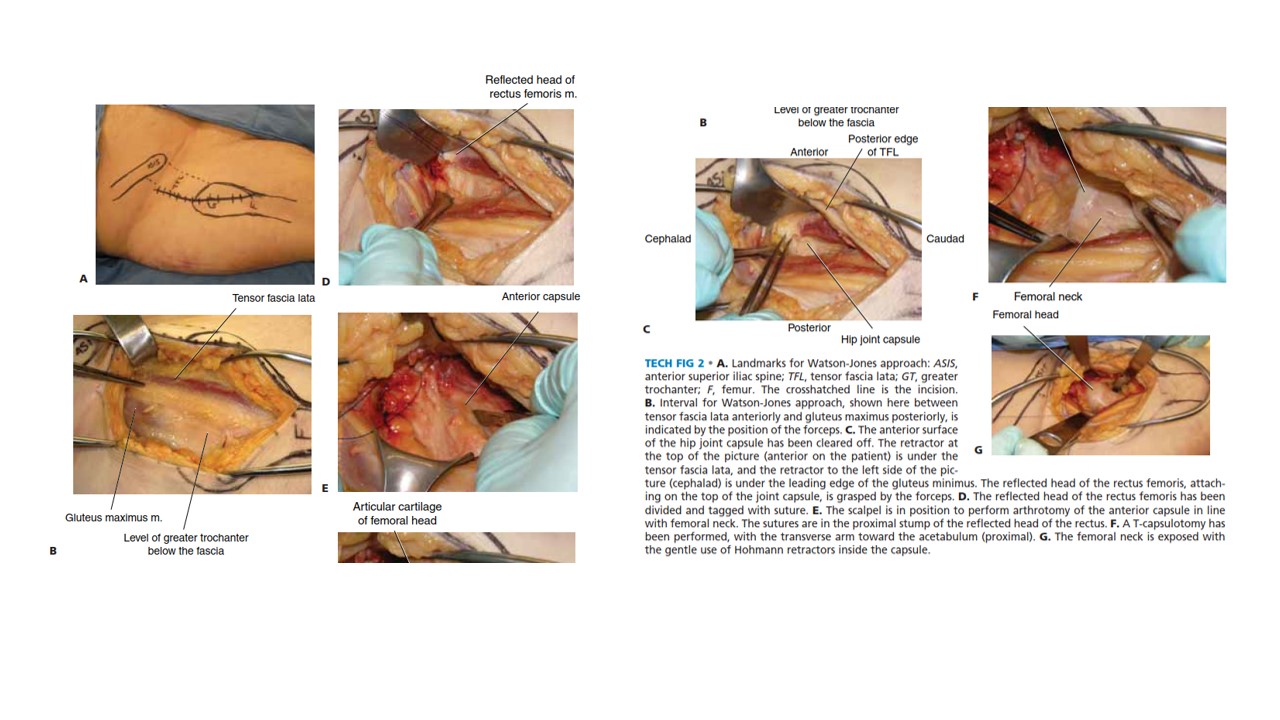
OPEN REDUCTION AND INTERNAL FIXATION THROUGH THE WATSON- JONES APPROACH
Fracture Reduction
TECH FIG 2 • A. Landmarks for Watson-Jones approach: ASIS, anterior superior iliac spine; TFL, tensor fascia lata; GT, greater trochanter; F, femur. The crosshatched line is the incision. B. Interval for Watson-Jones approach, shown here between tensor fascia lata anteriorly and gluteus maximus posteriorly, is indicated by the position of the forceps. C. The anterior surface of the hip joint capsule has been cleared off. The retractor at the top of the picture (anterior on the patient) is under the G tensor fascia lata, and the retractor to the left side of the pic- ture (cephalad) is under the leading edge of the gluteus minimus. The reflected head of the rectus femoris, attach- ing on the top of the joint capsule, is grasped by the forceps. D. The reflected head of the rectus femoris has been divided and tagged with suture. E. The scalpel is in position to perform arthrotomy of the anterior capsule in line with femoral neck. The sutures are in the proximal stump of the reflected head of the rectus. F. A T-capsulotomy has been performed, with the transverse arm toward the acetabulum (proximal). G. The femoral neck is exposed with the gentle use of Hohmann retractors inside the capsule.
Screw Placement
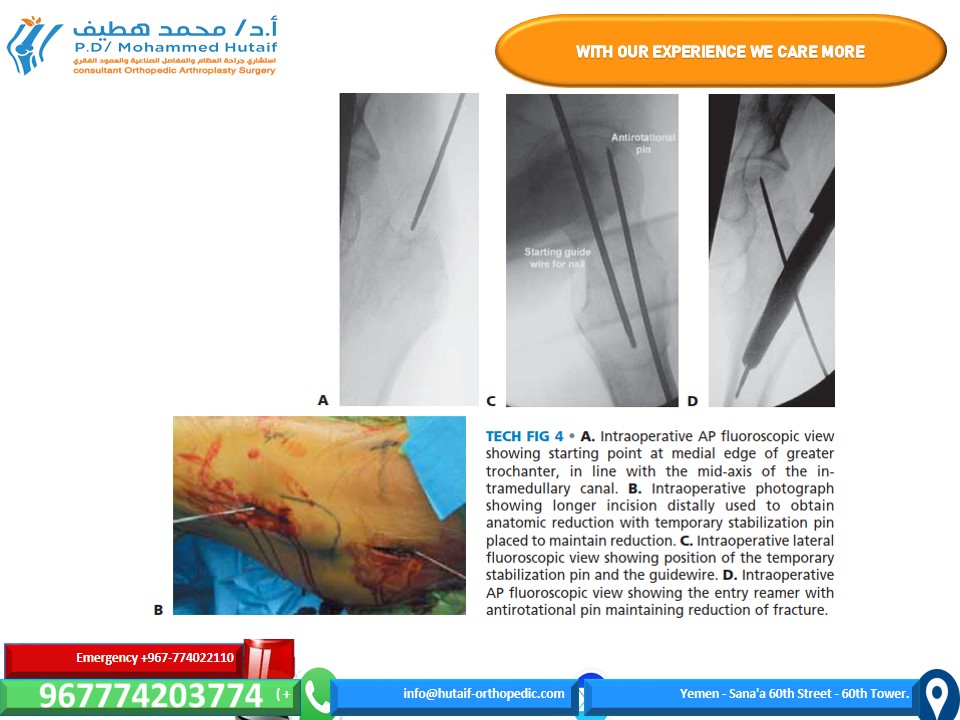
CEPHALOMEDULLARY NAIL FIXATION

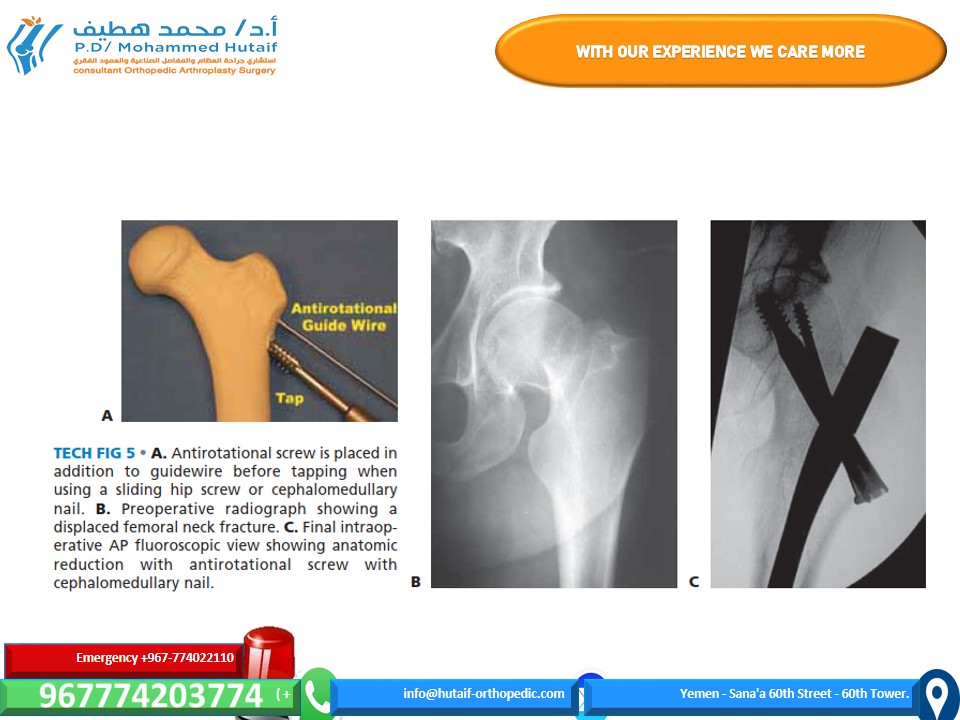
MINIMALLY INVASIVE FIXATION WITH A SLIDING HIP SCREW
Positioning, Reduction, and
Guidewire Placement