For Doctors Proximal Humeral Fractures Greater Tuberosity, Nondisplaced
Extraarticular 2-Part, Greater Tuberosity, Nondisplaced
1. General considerations
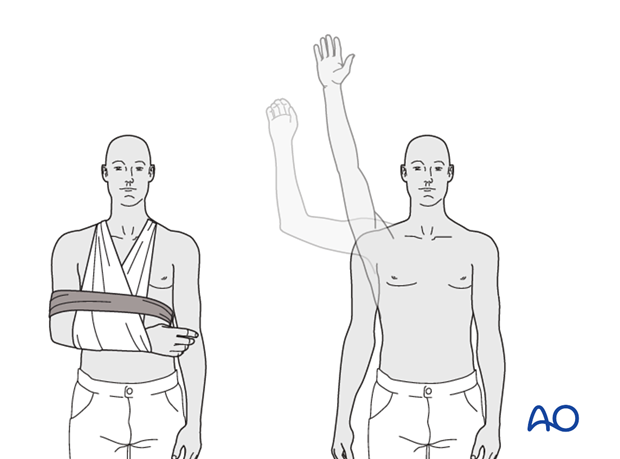
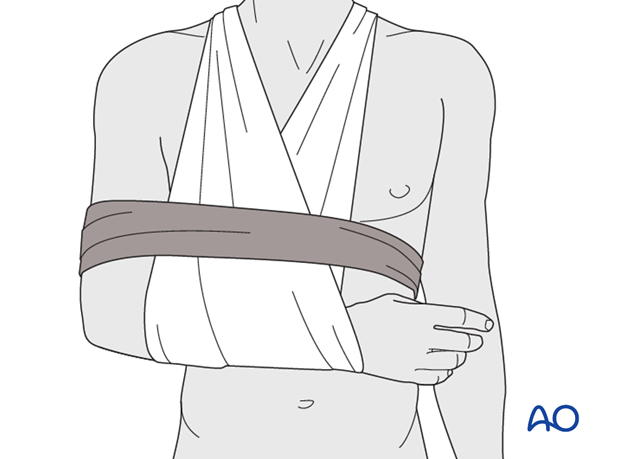
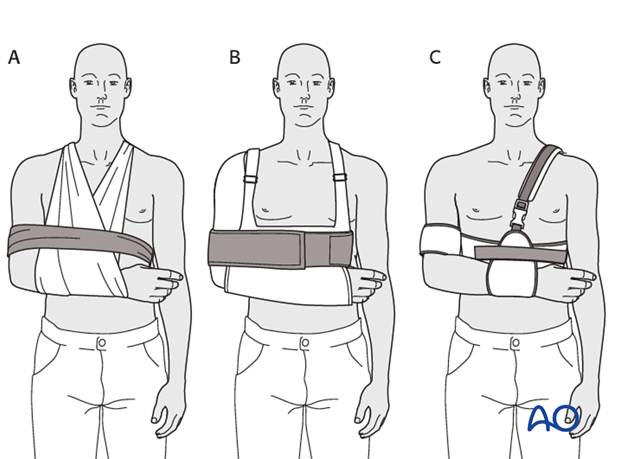
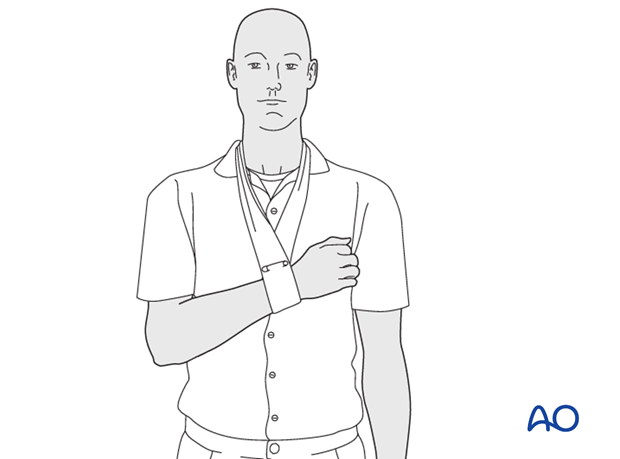
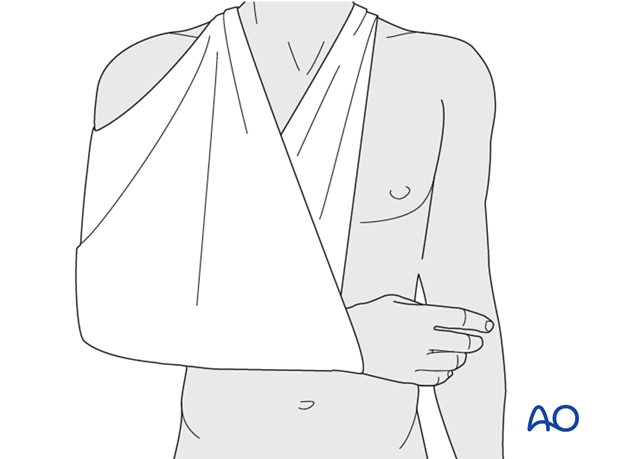
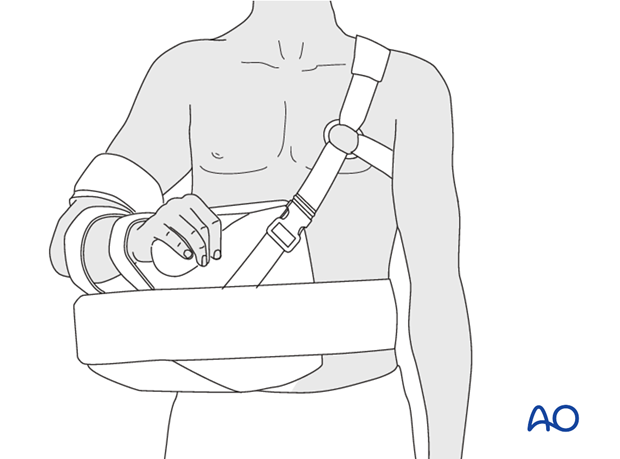
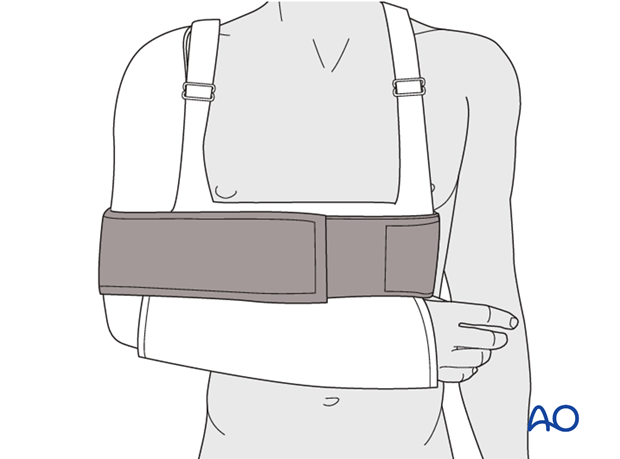
2. Sling and swath
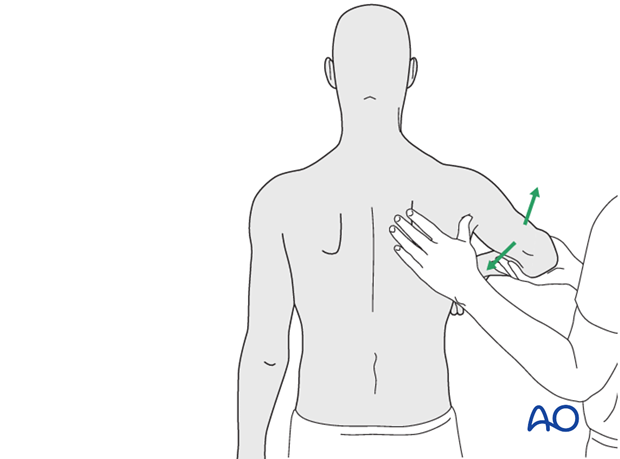
Optimal shoulder immobilization is achieved when the upper arm and forearm are secured to the chest. Traditionally, this has been done with a sling that supports the elbow and forearm and counteracts the weight of the arm. The simplest sling is a triangular bandage tied behind the neck.
Additional support is provided by a swath which wraps around the humerus and the chest to restrict shoulder motion further, and keep the arm securely in the sling.
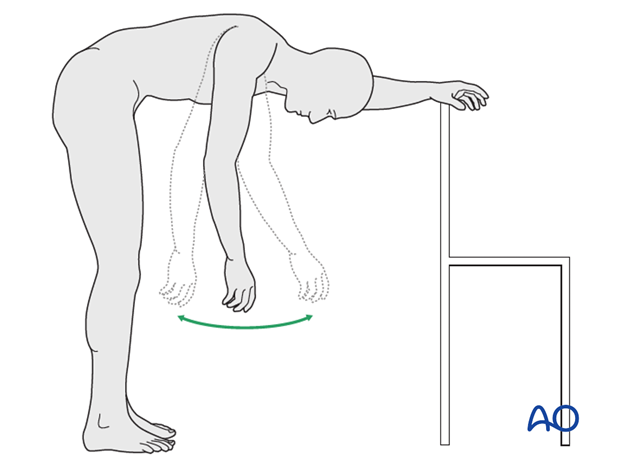
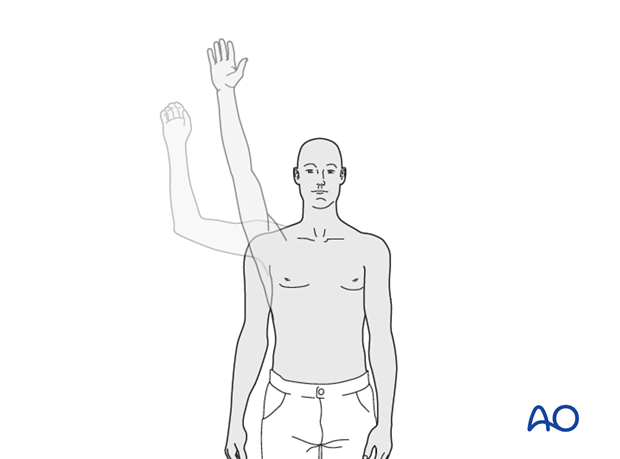
7. Mobilization: 2-3 weeks posttrauma
9. Shoulder therapy set: 3-6 weeks postoperative
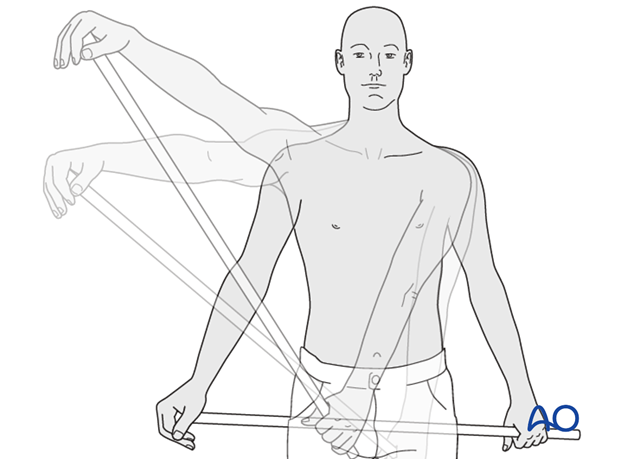
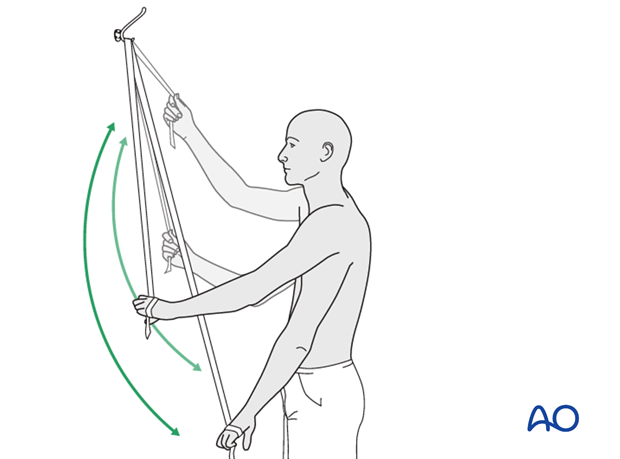
A “shoulder therapy set” might be helpful. Typically included devices are:
1) An exercise bar, which lets the patient use the uninjured left shoulder to passively move the affected right side.
2) A rope and pulley assembly. With the pulley placed above the patient, the unaffected left arm can be used to provide full passive forward flexion of the injured right shoulder.
12. Overview of rehabilitation
Special considerations
Glenohumeral dislocation: Use of a sling or sling-and-swath device, at least intermittently, is more comfortable for patients who have had an associated glenohumeral dislocation. Particularly during sleep, this may help avoid a redislocation.
Weight bearing: Neither weight bearing nor heavy lifting are recommended for the injured limb until healing is secure.
Implant removal: Implant removal is generally not necessary unless loosening or impingement occurs. Implant removal can be combined with a shoulder arthrolysis, if necessary.
Shoulder rehabilitation protocol
Phase 1 (approximately first 3 weeks)
- Immobilization and/or support for 2-3 weeks
- Pendulum exercises
- Gently assisted motion
- Avoid external rotation for first 6 weeks