Fracture patterns and their significance: Hair-line fractures
Fracture patterns and their significance: Hair-line fractures
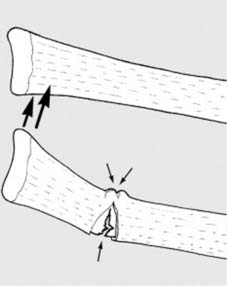
12 Pathological fractures (b): Pathological fractures may also occur at the site of simple tumours, e.g. a fracture of the humerus (a) in a child with a simple bone cyst (b). The commonest causes of pathological fracture are osteoporosis and osteomalacia.
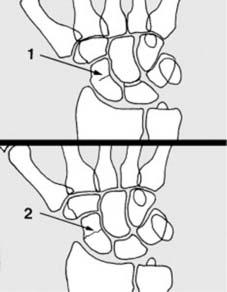
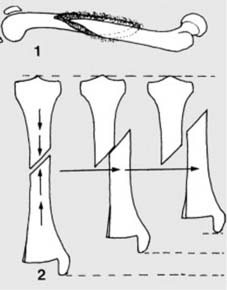
13 Fracture patterns and their significance: Hair-line fractures (a): Hair-line fractures result from minimal trauma, i.e. trauma which is just great enough to produce a fracture but not severe enough to produce any significant displacement of the fragments. Such fractures may be (1) incomplete or (2) complete.
14 Hair-line fractures (b): These fractures may be difficult to detect on the radiographs, and where there are reasonable clinical grounds for suspecting a fracture, the rules are quite clear. 1. Additional oblique radiographic projections of the area may be helpful. 2. Do not accept poor quality films. 3. Films repeated after 7–10 days may show the fracture quite clearly (due to decalcification at the fracture site). 4. A CT scan may also help confirm the diagnosis.
15 Hair-line fractures (c): Stress fractures are generally hair-line in pattern, and are often not diagnosed with certainty until there is a wisp of subperiosteal callus formation, or increased density at the fracture site some 3–6 weeks after the onset of symptoms. Where strongly suspected an MRI or bone scan may be helpful. Hair-line fractures generally heal rapidly requiring only symptomatic treatment: but the scaphoid and femoral neck are notable exceptions.
16 Hair-line fractures (d): Radiograph of upper tibia of an athletic adolescent with a 7-week history of persistent leg pain. Previous radiographs were reported as normal. Note the coned view to obtain optimal detail and the incomplete hair-line fracture revealed by bone sclerosis and subperiosteal callus. A crepe bandage support only was prescribed, and the symptoms settled in a further 6 weeks.
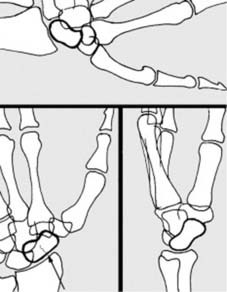
17 Greenstick fractures (a): Greenstick fractures occur in children, but not all children’s fractures are of this type. The less brittle bone of the child tends to buckle on the side opposite the causal force. Tearing of the periosteum and of the surrounding soft tissues is often minimal.
18 Greenstick fractures (b): This radiograph illustrates a more severe greenstick fracture of the distal radius and ulna. Note that although there is about 45° of angulation at the fracture site, there is no loss of bony contact in either fracture. The clinical deformity is clearly suggested by the soft-tissue shadow.
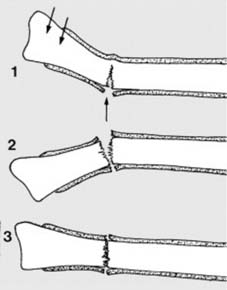
19 Greenstick fractures (c): Reduction of a greenstick fracture is facilitated by the absence of displacement and by the intact tissues on the concavity of the fracture. Angulation may be corrected by supporting the fracture and applying pressure over the distal fragment (1 and 2). The elastic spring of the periosteum may however lead to recurrence of angulation (3). Particular attention must therefore be taken over plaster fixation and after care.
20 Greenstick fractures (d): In the forearm in particular, where angulation inevitably leads to restriction of pronation and supination, some surgeons deliberately overcorrect the initial deformity (1). This tears the periosteum on the other side of the fracture (2). This reduces the risks of secondary angulation (3). Healing in all greenstick fractures is rapid.
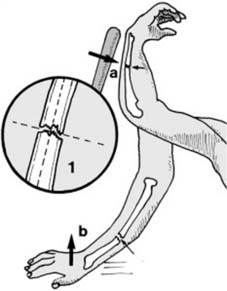
21 Simple transverse fractures (a): Transverse fractures run either at right angles to the long axis of a bone (1), or with an obliquity of less than 30°. They may be caused by direct violence, when the bone fractures directly beneath the causal force (e.g. the ulna fracturing when warding off a blow (a)). They may also result from indirect violence when the bone is subjected to bending stresses by remotely applied force (e.g. a fracture of the forearm bones resulting from a fall on the outstretched hand (b)).
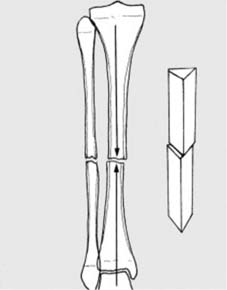
22 Simple transverse fractures (b): The inherent stability of this type of fracture (illustrated by the model on the right) reduces the risks of shortening and displacement. In the tibia, as a result, weight bearing may be permitted at a comparatively early stage. On the other hand, the area of bony contact is small, requiring very strong union before any external support can be discarded. (NB: The term ‘simple’ used to describe this and the following fractures means that the fracture runs circumferentially round the bone with the formation of only two main fragments.)
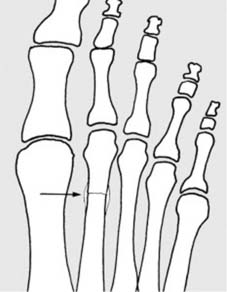
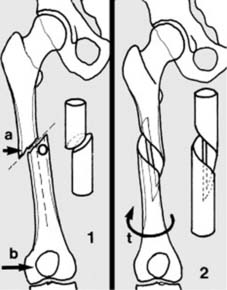
23 Simple oblique fractures (a): In an oblique fracture (1) the fracture runs at an oblique angle of 30° or more (O). Such fractures may be caused by (a) direct or (b) indirect violence. In simple spiral fractures (2) the line of the fracture curves round the bone in a spiral. Simple spiral fractures result from indirect violence, applied to the bone by twisting (torsional) forces (t).
24 Simple oblique and spiral fractures (b): In spiral fractures, union can be rapid (1) as there is often a large area of bone in contact. In both oblique and spiral fractures, unopposed muscle contraction or premature weight bearing readily lead to shortening, displacement and sometimes loss of bony contact (2). [Note: In the AO Classification of Fractures (see later) simple spiral, oblique and transverse fractures are classified as Type A fractures.]
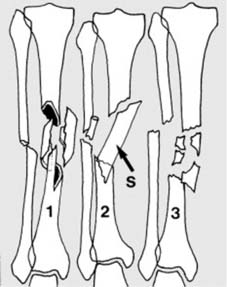
25 In multifragmentary (comminuted) fractures there are more than two fragments. The spiral wedge fracture (1) is produced by torsional forces (t), and the bending wedge fracture (2) by direct (a) or indirect (b) violence. The fragment (B) is often called a butterfly fragment (because of its shape). With greater violence a fragmented (comminuted) wedge fracture (3) results. [All these fractures are in Type B in the AO Classification (see later) and their characteristic is that after reduction there is still bony contact between the main fragments (4)].
26 In multifragmentary complex fractures (a further division of comminuted fractures) there is no contact between the main fragments after reduction. In complex spiral fractures (1) there are two or more spiral elements; in complex segmental fractures (sometimes called double fractures) (2) there is at least one quite separate complete bone fragment (S). In complex irregular fractures (3) the bone lying between the main elements is split into many irregular fragments. [All these fractures are classified as Type C in the AO Classification.]
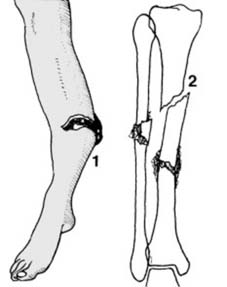
27 Multifragmentary fractures are generally the result of greater violence than is the case with most simple fractures, and consequently there is an increased risk of damage to neighbouring muscle, blood vessels and skin (1). The fractures tend to be unstable, and delayed union and joint stiffness are common. Segmental fractures are often difficult to reduce by closed methods, and direct exposure may threaten the precarious blood supply to the central segment. Non-union at one level is not uncommon in these fractures (2).
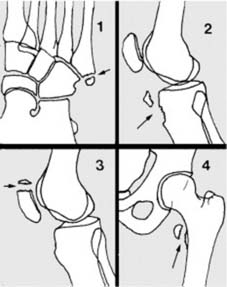
28 Impacted fractures: A fracture is impacted when one fragment is driven into the other (1). Cancellous bone is usually involved and union is often rapid. The stability of these fractures varies and is more implied than real. Displacement will occur if the fracture is subjected to deforming forces; e.g. without fixation, impacted femoral neck fractures frequently come adrift (2).
29 Compression (or crush) fractures: Crush fractures occur in cancellous bone which is compressed beyond the limits of tolerance. Common sites are (1) the vertebral bodies (as a result of flexion injuries) and (2) the heels (following falls from a height). If the deformity is accepted, union is invariably rapid. In the spine, if correction is attempted, recurrence is almost invariable.
30 Avulsion fractures (a): An avulsion fracture may be produced by a sudden muscle contraction, the muscle pulling off the portion of bone to which it is attached. Common examples include:
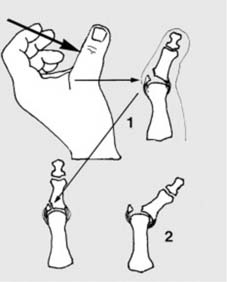
31 Avulsion fractures (b): Avulsion fractures may also result from traction on a ligamentous or capsular attachment: these are often witness of momentary dislocation; e.g. (1) an abduction force may avulse the ulnar collateral ligament attachment, with spontaneous reduction. Late subluxation (2) is common with this (‘gamekeeper’s thumb’) and other injuries and is especially serious in the case of the spine.
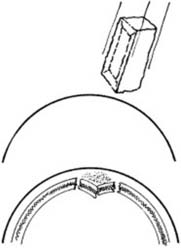
32 Depressed fracture: Depressed fractures occur when a sharply localised blow depresses a segment of cortical bone below the level of the surrounding bone. Although common in skull fractures, this pattern is only rarely found in the limbs. There the tibia in the upper third is probably most frequently affected. Healing is rapid; complications are dependent on the site.
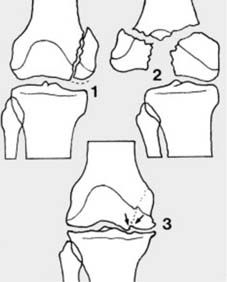
33 Fractures involving the articular surfaces of a joint: In partial articular fractures (1) part of the joint surface is involved, but the remainder is intact and solidly connected to the rest of the bone. (AO Type B fracture.) In complete articular fractures (2) the articular surface is completely disrupted and separated from the shaft. (AO Type C fracture.) When a fracture involves the articular surfaces, any persisting irregularity may cause secondary osteoarthritis (3). Stiffness is a common complication, and this may be minimised by early mobilisation.
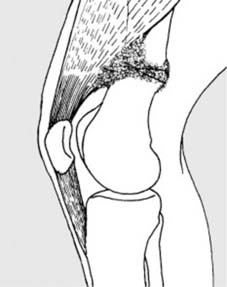
34 Fracture close to a joint: When a fracture lies close to a joint, stiffness may also be a problem due to tethering of neighbouring muscles and tendons by spread of callus from the healing fracture; e.g. in fractures of the femur close to the knee, the quadriceps may become bound down by the callus, resulting in difficulty with knee flexion.
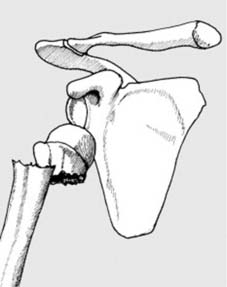
35 Fracture–dislocation: A fracture–dislocation is present when a joint has dislocated and there is in addition a fracture of one of the bony components of the joint. Illustrated is a fracture–dislocation of the shoulder, where there is an anterior dislocation with a fracture of the neck of the humerus. Injuries of this kind may be difficult to reduce and may be unstable. Stiffness and avascular necrosis are two common complications.
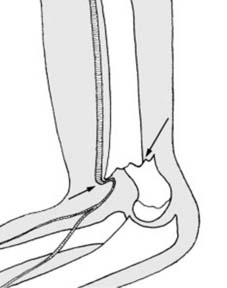
36 Complicated fractures: A fracture is described as complicated if there is accompanying damage to major neighbouring structures. The diagram is of a complicated supracondylar fracture of the humerus. (Such an injury might also be described as a supracondylar fractu