Clavicle Fractures
|
Clavicle Fractures
EPIDEMIOLOGYClavicle fractures account for approximately 2.6% of all fractures and for 44% to 66% of fractures about the shoulder. Middle third fractures account for 80% of all clavicle fractures, whereas fractures of the lateral and medial third of the clavicle account for 15% and 5%, respectively.. Clavicle Fractures
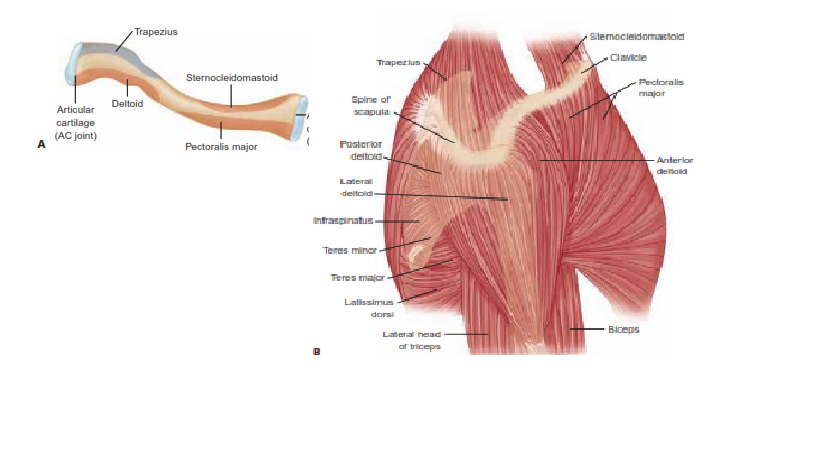
NATOMYThe clavicle is the first bone to ossify (fifth week of gestation) and the last ossification center (sternal end) to fuse, at 22 to 25 years of age. The clavicle is S-shaped, with the medial end convex forward and the lateral end concave forward. It is widest at its medial end and thins laterally. The medial and lateral ends have flat expanses that are linked by a tubular middle, which has sparse medullary bone. The clavicle functions as a strut, bracing the shoulder from the trunk and allowing the shoulder to function at optimal strength. The medial one-third protects the brachial plexus, the subclavian and axillary vessels, and the superior lung. It is strongest in axial load. The junction between the two cross-sectional configurations occurs in the middle third and constitutes a vulnerable area to fracture, especially with axial loading. Moreover, the middle third lacks reinforcement by muscles or ligaments distal to the subclavius insertion, resulting in additional vulnerability. The distal clavicle contains the coracoclavicular ligaments. The two components are the trapezoid and conoid ligaments. They provide vertical stability to the acromioclavicular (AC) joint. They are stronger than the AC ligaments.. Clavicle Fractures
MECHANISM OF INJURYFalls onto the affected shoulder leading to a bending force account for most (87%) of clavicular fractures, with direct impact accounting for only 7% and falls onto an outstretched hand accounting for 6%. Although rare, clavicle fractures can occur secondary to muscle contractions during seizures or secondary to minimal trauma due to pathologic bone or as stress fractures.. |
Clavicle Fractures
CLINICAL EVALUATIONPatients usually present with splinting of the affected extremity, with the arm adducted across the chest and supported by the contralateral hand to unload the injured shoulder. A careful neurovascular examination is necessary to assess the integrity of neural and vascular elements lying posterior to the clavicle. The proximal fracture end is usually prominent and may tent the skin. Assessment of skin integrity is essential to rule out open fracture. The chest should be auscultated for symmetric breath sounds. Tachypnea may be present as a result of pain with inspiratory effort; this should not be confused with diminished breath sounds, which may be present from an ipsilateral pneumothorax caused by an apical lung injury
Clavicle Fractures
ASSOCIATED INJURIESUp to 9% of patients with clavicle fractures have additional fractures, most commonly rib fractures. Most brachial plexus injuries are associated with proximal third clavicle fractures (traction injury). The skin is often abraded as a result of the injury mechanism.. Clavicle Fractures
RADIOGRAPHIC EVALUATIONStandard anteroposterior radiographs are generally sufficient to confirm the presence of a clavicle fracture and the degree of fracture displacement. A 30-degree cephalad tilt view provides an image without the overlap of the thoracic anatomy. An apical oblique view can be helpful in diagnosing minimally displaced fractures, especially in children. This view is taken with the involved shoulder angled 45 degrees toward the xray source, which is angled 20 degrees cephalad. A chest x-ray allows for side-to-side comparison, including normal length. Computed tomography may be useful, especially in proximal third fractures, to differentiate sternoclavicular dislocation from epiphyseal injury, or in distal third fractures, to identify if there was articular involvement.. |
|
CLASSIFICATION
DESCRIPTIVE
Clavicle fractures can be classified according to anatomic description, including location, displacement, angulation, pattern (e.g., greenstick, oblique, transverse), and comminution.
ALLMAN
Group I: fracture of the middle third (80%). This is the most common fracture in both children and adults; proximal and distal segments are secured by ligamentous and muscular attachments (Fig. 11.1).
FIGURE 11.1 Radiograph of a displaced middle third clavicle fracture.
Group II: fracture of the distal third (15%). This is subclassified according to the location of the coracoclavicular ligaments relative to the fracture (Fig. 11.2):
Type I: Minimal displacement: interligamentous fracture between the conoid and trapezoid or between the coracoclavicular and AC ligaments; ligaments still intact
Type II: Displaced secondary to a fracture medial to the coracoclavicular ligaments: higher incidence of nonunion
IIA: Conoid and trapezoid attached to the distal segment
IIB: Conoid torn, trapezoid attached to the distal segment
Type III: Fracture of the articular surface of the AC joint with no ligamentous injury: may be confused with first-degree AC joint separation
FIGURE 11.2 Classification of group II clavicle fractures. Type I: Fracture is nondisplaced. Type IIA: Both conoid and trapezoid ligaments are on distal segment, and proximal segment without ligamentous attachments is displaced. Type IIB: Conoid ligament is ruptured, trapezoid ligament remains attached to the distal segment, and proximal fragment is displaced. Type III: Distal clavicle fracture, involving only the articular surface of the AC joint; no ligamentous disruption or displacement occurs. These fractures present as late degenerative changes of the joint. (Adapted from Sajadi KR. Clavicle fractures: epidemiology, clinical evaluation, imaging, and classification. In: Ianotti JP, Miniaci A, Williams GR Jr, et al., eds. Disorders of the Shoulder: Diagnosis and Management: Shoulder Trauma. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2014:99–107.)
Group III: fracture of the proximal third (5%). Minimal displacement results if the costoclavicular ligaments remain intact. It may represent epiphyseal injury in children and teenagers. Subgroups include:
Type I: Minimal displacement
Type II: Displaced
Type III: Intra-articular
Type IV: Epiphyseal separation
Type V: Comminuted
ORTHOPAEDIC TRAUMA ASSOCIATION CLASSIFICATION OF CLAVICLE FRACTURES
See Fracture and Dislocation Classification Compendium at:
https://ota.org/research/fracture-and-dislocation-compendium
TREATMENT
NONOPERATIVE
Most minimally displaced clavicle fractures can be successfully treated nonoperatively with some form of immobilization.
Comfort and pain relief are the main goals. A sling has been shown to provide the same results as a figure-of-eight bandage, providing more comfort and fewer skin problems. The goals of the various methods of immobilization are as follows:
To support the shoulder girdle, raising the lateral fragment in an upward, outward, and backward direction (sling)
To depress the medial fragment (figure of eight)
To maintain some degree of fracture reduction (both)
To allow for the patient to use the ipsilateral hand and elbow
Regardless of the method of immobilization utilized, some degree of shortening and deformity usually result.
In general, immobilization is used for 4 to 6 weeks.
During the period of immobilization, active range of motion of the elbow, wrist, and hand should be performed.
OPERATIVE
The surgical indications for midshaft clavicle fractures have become more standard in the past 20 years.
The accepted indications for operative treatment of acute clavicle fractures are open fracture, associated neurovascular compromise, and skin tenting with the potential for progression to open fracture.
Controversy exists over management of midshaft clavicle fractures with substantial displacement (more than 100%), comminution (Z deformity), and shortening (>1 to 2 cm).
Although most displaced midshaft fractures will unite, studies have reported shoulder dysfunction and patient dissatisfaction with the resulting cosmetic deformity.
There is also more recent evidence that functional outcome may be improved in some of these patients with surgical treatment. Furthermore, the presence of a malunion may portend inferior function.
Controversy also exists over management of type II distal clavicle fractures.
Some authors have indicated that all type II fractures require operative management due to high rate of nonunion.
Others report that if the bone ends are in contact, healing can be expected even if there is some degree of displacement. In this situation, nonoperative management consists of sling immobilization and progressive range of shoulder motion.
Operative fixation may be accomplished via the use of:
Plate fixation: This is placed either on the superior or on the anteroinferior aspect of the clavicle.
Plate and screw fixation requires a more extensive exposure than intramedullary devices but has the advantage of more secure fixation counteracting tensile forces. Plate and screw fixation may be prominent, particularly if placed on the superior aspect of the clavicle.Adjunctive suture fixation (substitution) of the coracoclavicular ligaments may be helpful for distal fractures with limited area for screw purchase.
Newer low-profile implants and/or anteroinferior placement may preclude this finding.Intramedullary fixation: usually placed in retrograde fashion through the lateral fragment and then in anterograde fashion into the medial fragment or antegrade as a flexible implant that is then stiffenedUse of intramedullary fixation requires frequent radiographic follow-up to monitor the possibility of hardware migration and a second procedure for hardware removal.Older intramedullary pins are prone to skin erosion at the hardware insertion site laterally. Historically, these implants have been reported to be associated with complications in up to 50% of cases.
Operative treatment of type II distal clavicle fractures consists of reducing the medial fragment to the lateral fragment. This is accomplished by using either coracoclavicular fixation (Mersilene tape, sutures, wires, or screws) or fixation across the AC joint, through the lateral fragment and into the medial fragment (lateral clavicle plates).
COMPLICATIONS
Neurovascular compromise: This is uncommon and can result from either the initial injury or secondary to compression of adjacent structures by callus and/or residual deformity.
Subclavian vessels are at risk with superior plating.
Malunion: This may cause a bony prominence, and resultant shortening may be associated with poorer Disabilities of the Arm, Shoulder and Hand (DASH) scores at 1 year.
Nonunion: The incidence of nonunion following clavicle fractures ranges from 0.1% to 13.0%, with 85% of all nonunions occurring in the middle third. Factors that have been implicated in the development of nonunions of the clavicle include:
Severity of initial trauma (open wound)
Extent of initial displacement of fracture fragments Soft tissue interposition
Refracture
Inadequate period of immobilization Primary open reduction and internal fixation
Posttraumatic arthritis: This may occur after intra-articular injuries to the sternoclavicular or AC joint.
Intramedullary Fixation of Clavicle Fractures
DEFINITION
ANATOMY
PATHOGENESIS
NATURAL HISTORY
PATIENT HISTORY AND PHYSICAL FINDINGS
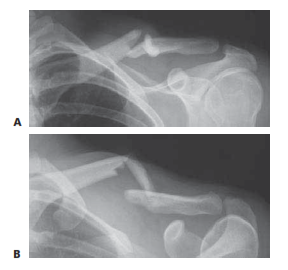 FIG 3 • Radiographs of the same displaced left clavicle fracture viewed from a standard AP projection (A) and a 45-degree cephalic tilt projection (B).
FIG 3 • Radiographs of the same displaced left clavicle fracture viewed from a standard AP projection (A) and a 45-degree cephalic tilt projection (B).IMAGING AND OTHER DIAGNOSTIC STUDIES
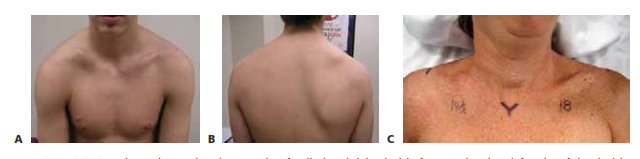 FIG 2 • A,B. Anterior and posterior photographs of a displaced right clavicle fracture showing deformity of the clavicle and drooping of the shoulder girdle downward and forward. C. Clinical picture of a displaced right clavicle fracture, showing 3.5 cm of shortening, measured from the sternal notch to the acromioclavicular joint.
FIG 2 • A,B. Anterior and posterior photographs of a displaced right clavicle fracture showing deformity of the clavicle and drooping of the shoulder girdle downward and forward. C. Clinical picture of a displaced right clavicle fracture, showing 3.5 cm of shortening, measured from the sternal notch to the acromioclavicular joint.DIFFERENTIAL DIAGNOSIS
NONOPERATIVE MANAGEMENT
SURGICAL MANAGEMENT
INCISION AND DISSECTION
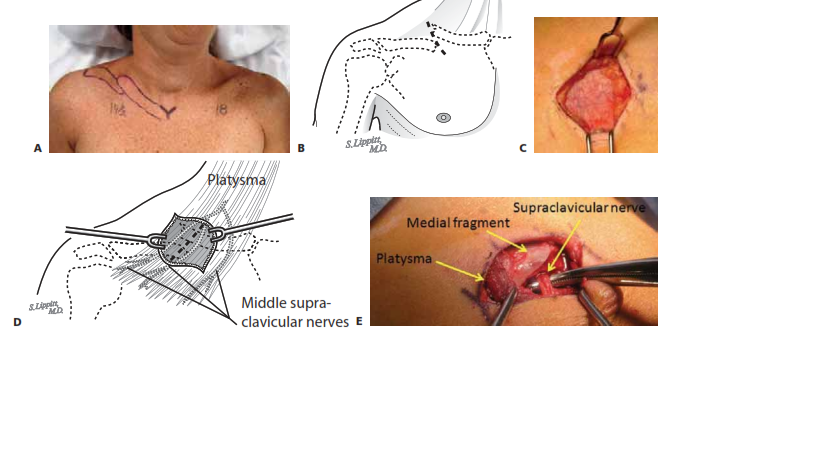
CLAVICLE PREPARATION
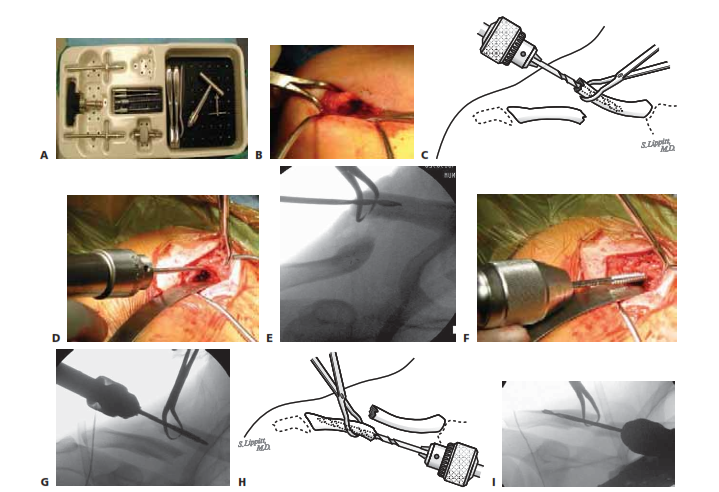
 K
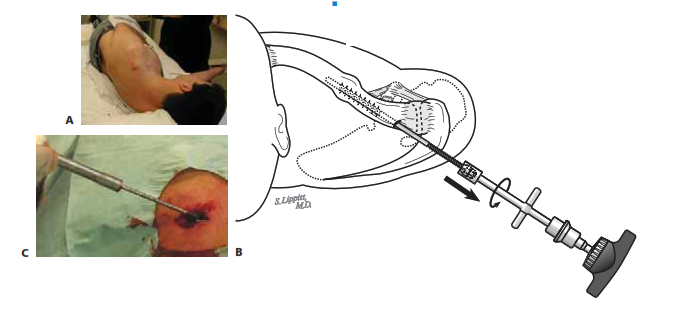
KPIN INSERTION AND FRACTURE REDUCTION
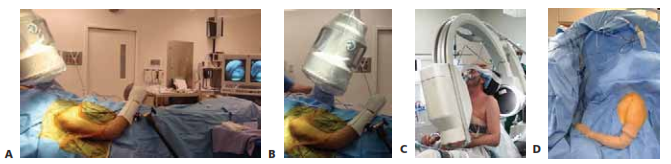
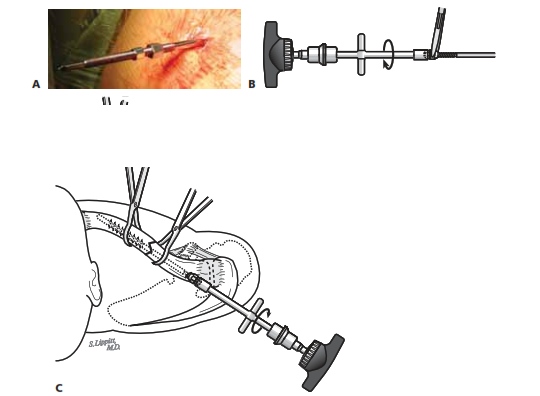
 TECH FIG 3 • A. The surgeon continues firmly holding the lateral fragment while passing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the pos- terolateral cortex. Once just through the cortex, the surgeon makes a small incision
TECH FIG 3 • A. The surgeon continues firmly holding the lateral fragment while passing the trocar end (lateral end) of the clavicle pin into the intramedullary canal, out the previously drilled hole in the pos- terolateral cortex. Once just through the cortex, the surgeon makes a small incisionB
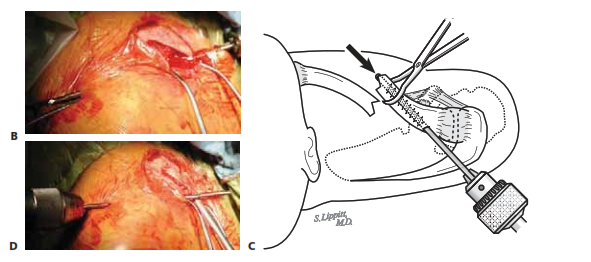
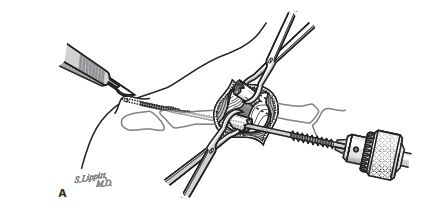
FINAL POSITIONING OF PIN AND FRACTURE COMPRESSION
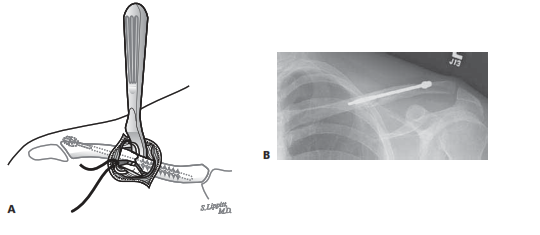
 TECH FIG 4 • A. The lateral end of the pin with the larger medial nut is placed first, closest to the skin, followed by the smaller lat- eral nut, in preparation for cold welding. B. To cold weld the joint, the medial nut is grasped with a needle-nose pliers, and then the lateral nut is tightened against the medial nut using the lateral nut wrench. C. Using the lateral nut wrench and C-arm guidance, the surgeon advances the pin assembly into the medial fragment until it contacts the an-
TECH FIG 4 • A. The lateral end of the pin with the larger medial nut is placed first, closest to the skin, followed by the smaller lat- eral nut, in preparation for cold welding. B. To cold weld the joint, the medial nut is grasped with a needle-nose pliers, and then the lateral nut is tightened against the medial nut using the lateral nut wrench. C. Using the lateral nut wrench and C-arm guidance, the surgeon advances the pin assembly into the medial fragment until it contacts the an-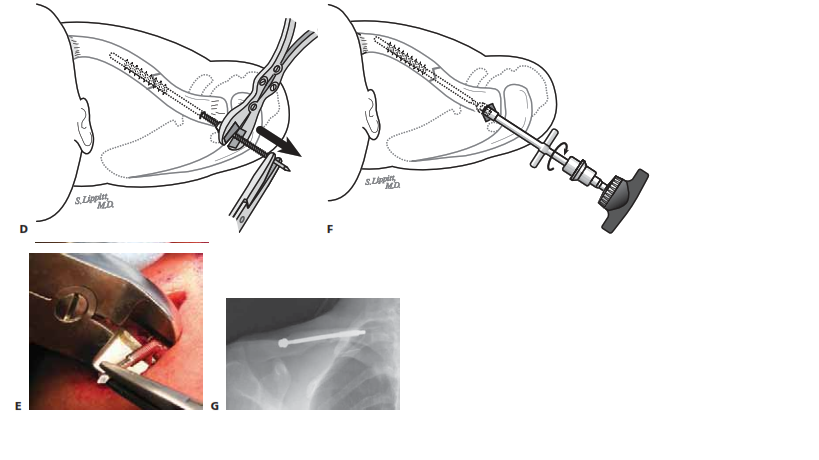
BUTTERFLY FRAGMENT MANAGEMENT AND WOUND CLOSURE
PIN REMOVAL
PEARLS AND PITFALLS
POSTOPERATIVE CARE


